Sepsis Coding
Published On - August 12, 2020
ICD-10-CM Sepsis
Coding
Sepsis
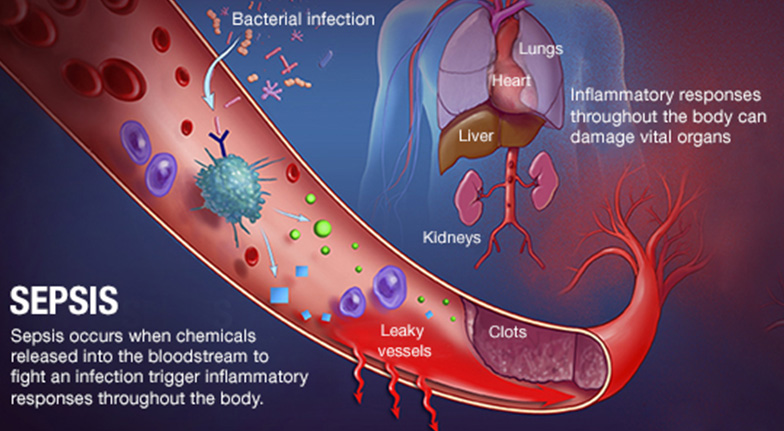
is a life-threatening complication that develops when the chemicals the immune
system releases into the bloodstream to fight an infection cause inflammation
throughout the body instead. Coding of Sepsis and Severe Sepsis can be
complicated and physicians would do well to rely on medical coding services to report these
conditions. Experienced coders carefully review ICD-10 guidelines and clinical
documentation to assign the right codes for sepsis, severe sepsis and septic
shock.
Physicians
should use the term “bacteremia” if there is evidence of bacteria circulating
in the blood. Since ICD-10 utilizes combination coding, sepsis without acute
organ failure requires only one code, that is, the code for the underlying
systemic infection (A40.0 – A41.9). Complete and accurate coding of severe
sepsis, however, requires a combination of at least two codes – the first code
sequenced to identify the underlying organism (Sepsis, A40.0 – A41.9) or cause
of the sepsis (postprocedural infection, trauma, or burn), followed by a code
indicating the extent to which the septic condition has progressed, that is,
severe sepsis with or without septic shock.
Sepsis
- If the
underlying infection or causative organism is not further specified, code
A41.9, Sepsis unspecified organism should be assigned.
- For a diagnosis
of sepsis, the appropriate code for the underlying systemic infection
should be assigned, for instance, A41.51 (Sepsis due to Escherichia coli).
One combination code is used to capture the underlying systemic infection
and the body’s inflammatory response to it.
- A code from
subcategory R65.2, Severe sepsis, should not be assigned unless severe
sepsis or an associated acute organ dysfunction is documented.
ICD-10
guidelines state that the coder should query the provider in the following
instances:
- If the blood
culture is negative or inconclusive, as this does not rule out the
presence of sepsis.
- If the term
‘urosepsis’ is used in the documentation, as urosepsis is not considered
synonymous with sepsis.
- If the
documentation is not clear as to whether an acute organ dysfunction is
related to the sepsis or another medical condition.
If
it is reported that the patient has sepsis and associated acute organ
dysfunction or multiple organ dysfunction (MOD), the instructions for coding
severe sepsis should be followed.
Severe Sepsis
R65.2,
Severe sepsiswithout septic shock
Severe
sepsis is a result of both community-acquired and health care-associated
infections. It is reported that pneumonia accounts for about half of all cases
of severe sepsis, followed by intraabdominal and urinary tract infections.
A
minimum of two codes are needed to code severe sepsis. First, an appropriate
code has to be selected for the underlying infection, such as, A41.51 (Sepsis
due to Escherichia coli), and this should be followed by code R65.2, severe
sepsis.
- If the causal
organism is not documented, code A41.9, Sepsis, unspecified organism,
should be assigned for the infection.
- An additional
code should be assigned for the organ dysfunction severe sepsis is
causing, such as, N17.0 Acute kidney failure with tubular necrosis.
- If a patient has
sepsis and an acute organ dysfunction, but the medical record
documentation indicates that the acute organ dysfunction is related to a
medical condition other than the sepsis, a code from subcategory R65.2,
Severe sepsis should not be assigned.
- The provider
should be queried if the documentation is not clear as to whether an acute
organ dysfunction is related to the sepsis or another medical condition.
Septic Shock
R65.21,
Severe sepsis with septic shock
As
it typically refers to circulatory failure associated with severe sepsis,
septic shock indicates a type of acute organ dysfunction.
The
code for septic shock cannot be assigned as a principal diagnosis. For septic
shock, the code for the underlying infection should be sequenced first,
followed by code R65.21, Severe sepsis with septic shock or code T81.12,
Postprocedural septic shock. Additional codes are also required to report other
acute organ dysfunctions.
Sequencing of Severe Sepsis
- If severe
sepsis is present on admission, and meets the definition of a principal diagnosis,
the underlying systemic infection should be assigned as principal
diagnosis followed by the appropriate code from subcategory R65.2,
following the sequencing rules in the Tabular List. A code from
subcategory R65.2 can never be assigned as a principal diagnosis.
- If the severe
sepsis was not present on admission but develops during the encounter, the
underlying systemic infection and the appropriate code from subcategory
R65.2 (Severe sepsis) should be assigned as secondary diagnoses.
- It could happen
that severe sepsis is present on admission, but the diagnosis may not be
confirmed until sometime after admission. The provider should be queried
if the documentation is not clear whether severe sepsis was present on
admission.
Sepsis and Severe Sepsis with a Localized Infection
- If a
patient is admitted with both sepsis or severe sepsis and a localized
infection, such as pneumonia or cellulitis, a code(s) for the underlying
systemic infection should be assigned first and the code for the localized
infection should be reported as a secondary diagnosis.
- If severe sepsis
is present, a code from subcategory R65.2 should also be assigned as a
secondary diagnosis.
- If the reason
for the admission is a localized infection, such as pneumonia, and
sepsis/severe sepsis does not develop until after admission, the localized
infection should be reported first, followed by the appropriate
sepsis/severe sepsis codes.
Sepsis due to a Postprocedural
Infection
- Documentation of
causal relationship: The provider’s documentation of the relationship
between the infection and the procedure should determine code assignment.
- Sepsis due to a
postprocedural infection: For such cases, the postprocedural infection
code should be coded first, such as: T80.2, Infections following infusion,
transfusion, and therapeutic injection, T81.4, Infection following a
procedure, T88.0, Infection following immunization, or O86.0, Infection of
obstetric surgical wound. This should be followed by the code for the
specific infection. If the patient has severe sepsis, the appropriate code
from subcategory R65.2 should also be assigned with the additional code(s)
for any acute organ dysfunction.
- Postprocedural
infection and postprocedural septic shock: If the patient develops
postprocedural infection which has resulted in severe sepsis, the code for
the precipitating complication should be assigned first, such as, T81.4,
Infection following a procedure, or O86.0, Infection of obstetrical
surgical wound. This should be followed by code R65.20, Severe sepsis without
septic shock and a code for the systemic infection.
Sepsis and severe sepsis associated with a
noninfectious process (condition)
- If the physician
documents sepsis or severe sepsis as associated with a noninfectious
condition, such as a burn or serious injury, and this condition meets the
definition for principal diagnosis, the code for the noninfectious
condition should be assigned first, followed by the code for the resulting
infection. If severe sepsis is present, a code from subcategory R65.2 should
also be assigned with any associated organ dysfunction(s) codes.
- If the infection
meets the definition of principal diagnosis, it should be sequenced before
the non-infectious condition. If both the associated non-infectious
condition and the infection meet the definition of principal diagnosis,
either may be assigned as principal diagnosis.
- When a
non-infectious condition leads to an infection resulting in severe sepsis,
assign the appropriate code from subcategory R65.2, Severe sepsis.
- It is not necessary
to additionally assign a code from subcategory R65.1, Systemic
inflammatory response syndrome (SIRS) of non-infectious origin, when a
non-infectious condition leads to an infection resulting in severe sepsis.
Write a public review