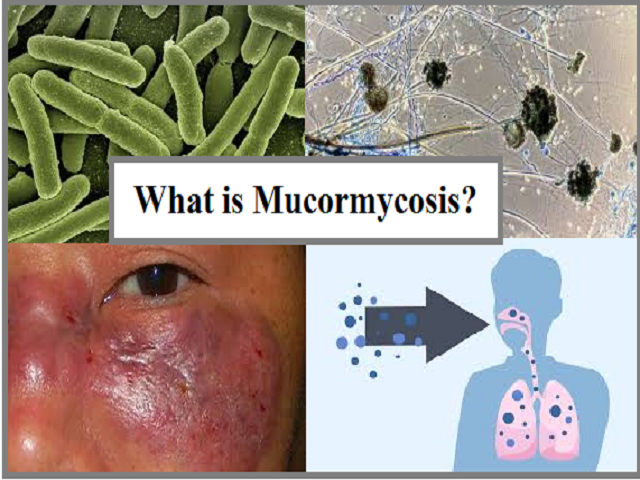
Mucormycosis - Symptoms & Treatment
Published On - May 20, 2021
Symptoms of
Mucormycosis
The
symptoms of mucormycosis depend on where in the body the fungus is growing.
Symptoms
of rhinocerebral (sinus and brain) mucormycosis include:
- One-sided facial
swelling
- Headache
- Nasal or sinus
congestion
- Black lesions on
nasal bridge or upper inside of mouth that quickly become more severe
- Fever
Symptoms
of pulmonary (lung) mucormycosis include:
- Fever
- Cough
- Chest pain
- Shortness of
breath
Cutaneous
(skin) mucormycosis
can look like blisters or ulcers, and the infected area may turn black. Other
symptoms include pain, warmth, excessive redness, or swelling around a wound.
Symptoms
of gastrointestinal mucormycosis include:
- Abdominal pain
- Nausea and vomiting
- Gastrointestinal
bleeding
Disseminated
mucormycosis
typically occurs in people who are already sick from other medical conditions,
so it can be difficult to know which symptoms are related to mucormycosis.
Patients with disseminated infection in the brain can develop mental status
changes or coma.
Also known as ‘black fungus’ or ‘mucormycosis’, it is a
rare kind of fungal infection affecting 1 in 10,00,000 people, but with an
overall mortality rate of 50 per cent. The disease is often characterized by
hyphae growing in and around blood vessels and can be potentially
life-threatening in diabetic or severely immunocompromized individuals.
“What is more worrying is
that the use of steroids for treating certain cases of COVID-19 would shoot up
sugar levels; this coupled with lack of physical activity puts diabetic people
at a higher risk of catching the black fungal infection,” the doctor warns.
According to doctors,
steroids reduce inflammation in the lungs due to COVID-19 and appear to help
curb some of the damage that can happen when the body’s immune system fights
against the virus. But, they also reduce immunity and push up blood sugar
levels in both diabetics and non-diabetic COVID-19 patients.
“For diabetes patients,
this is life-threatening. A person affected with mucormycosis may need early
detection and powerful diagnosis for treatment, which may, in turn, affect
other organs such as the kidneys. Prevention is extremely crucial,” Doctors say.
Write a public review