How to apply ICD-10-CM codes
Published On - April 02, 2020
Basically the ICD-10-CM book is divided into 2 sections: Alphabetical Index and Tabular List.
You will be coding diagnoses, illness, conditions, injury and external causes using ICD-10
You need to check the
disease/illness in the Alphabetical Index first. It will direct you to
the correct code. Once you go to the code in Tabular list read all the
rules for that code and then carefully choose the correct code. Quite a
simple process but just needs some attention!
ICD-10-CM Guidelines for Coding and Reporting
Guidelines for coding
and reporting with ICD-10-CM are provided by the Centers for Medicare
and Medicaid Services (CMS) and the National Center for Health
Statistics (NCHS). These guidelines have been approved by the four
organizations that make up the Cooperating Parties for the ICD-10-CM:
the American Hospital Association (AHA), the American Health Information
Management Association (AHIMA), CMS, and NCHS. The conventions of
ICD-10-CM take precedence over these guidelines, however.
Basic ICD-10-CM Coding Steps
Step 1: Locate the Code
To locate the code, the
coder must find the diagnosis, condition, or reason for visit in the
Alphabetic Index and verify the provided code in the Tabular List. The
coder has to follow all instructional notes
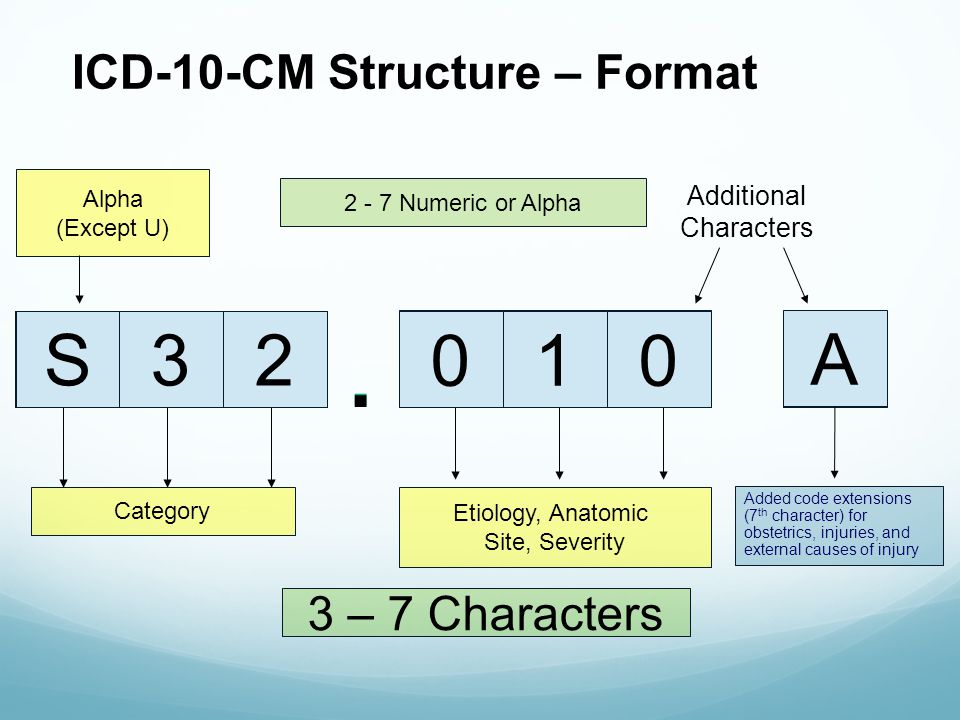
Step 2: Assign Code to the Highest Level
For maximum
reimbursement and to prevent claim denials, the coder must assign the
code to the highest level of detail. This is accomplished by:
- Assigning a three-character code only if there are no four-character codes listed.
- Assigning a four-character code only when there are no five-character codes in that subcategory.
- Assigning a five-character code only when there are no six-character codes in that subcategory.
- Assigning a six-character code when one such subclassification is provided.
- Assigning a seven-character code extension when provided
Step 3: Assign Residual Codes
The use of NEC and NOS
(residual codes) as appropriate involves using the main term entry in
the Alphabetic Index that is followed by a code number for the
unspecified condition. This code is never used when subterms exist that
allow for use of a more specific
Step 4: Assign Combination Codes
If available, the coder
should assign combination codes, which are codes used to classify either
two diagnoses with associated secondary process or a diagnosis with an
associated complication. Combination codes are listed in the Index and
contain connecting words such as "due to," "with," and "associated with"
Step 5: Assign Multiple Codes
Multiple coding is the
use of more than one code for the identification of certain elements of a
complex diagnostic or procedural statement. These statements connect
words and phrases by using "with," "incidental to," and "secondary to."
Special circumstances related to multiple coding include:
· Mandatory multiple
coding – This type of coding is used for "dual classification," which
describes the required assignment of two codes to give information about
manifestations and/or characteristics and the associated underlying
condition, disease, and/or etiology. These codes are found in the
Alphabetic Index by the use of a second code listed in brackets.
· Discretionary
multiple coding – This type of coding involves "code first" notes that
appear in the Tabular List. These notes are under certain codes that are
not specifically manifestation or characteristic codes, but codes in
which the condition may be due to the underlying condition, disease,
illness, or cause. The underlying condition should be always sequenced
first with these codes.
Example: Malignant
ascites (R18.0) has a note that specifies "code first" the malignancy,
such as malignant neoplasm of ovary (C56.-). For this encounter, code
C56.- would be listed first, followed by code R18.0.
· Indiscriminate
multiple coding – The coder should avoid indiscriminate coding of
irrelevant information, such as codes for characteristics of the
diagnosis and codes based on findings of diagnostic tests unless
confirmed by the physician.
Step 6: Code Unconfirmed Diagnosis
For inpatient admissions
that are listed as "possible," "probable," or "questionable," the coder
should report as though the diagnosis was established. The exception to
this step is when coding HIV infection and influenza due to certain
identified viruses, such as avian flu or H1N1 virus
Coders should report the
CPT code for closed treatment of the fracture only, because cast application is
integral to any definitive fracture treatment. The physician may report
supplies with the appropriate Q codes.
If the closed reduction had
been performed in the emergency department, the facility would only assign
codes for the treatment and the supply, if applicable, but not for the
application of the cast.
Signs and Symptoms
(ICD)
Codes that describe
symptoms and signs, as opposed to diagnoses, are acceptable for reporting only
when a definitive diagnosis has not been established. When definitive diagnosis
has been documented, do not code symptoms.
Personal History of malignancy (Z85)
You should use a personal
history Z code only when documentation shows there is no evidence of the
primary malignancy AND the patient
is no longer receiving treatment aimed at that site.
Diabetes Type
(ICD)
If the type of diabetes
mellitus is not documented the default is E11 – Diabetes Mellitus Type 2.
Dominant vs. Nondominant side
For ambidextrous patients,
the default is dominant
If the left side is
affected, the default is nondominant
If the right side is
affected, the default is dominant.
Sequela (Late Effects)
A sequela is the residual effect (condition
produced) after the acute phase of an illness or injury has terminated. There
is no time limit on when a
sequela code can be used.
Place holder X
If a code that requires a 7th character is not 6
characters, a placeholder X must be used to fill in the empty characters.
Displaced vs. Non displaced fracture coding (ICD)
In ICD-10-CM a fracture
not indicated as displaced or nondisplaced should be coded to displaced,
and a fracture not designated as open or closed should be coded to closed. While the
classification defaults to displaced for fractures, it is very important that
complete documentation is encouraged.
Write a public review